After this engaging session, radiology participants who said they would plan on regularly reporting BAC as part of their mammogram readings jumped from 50% to 95%!
Watch now to find out why.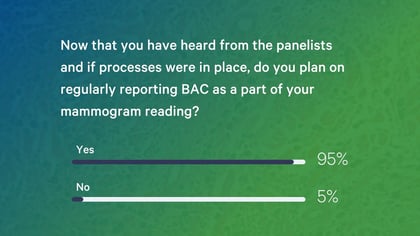
Recent advances in artificial intelligence (AI) have made it possible for doctors to detect breast cancers earlier and more accurately, all while reducing false positives and sparing patients the stress of unnecessary recalls. But while breast cancer is an incredibly serious, deadly disease, it is actually not the number one cause of death for women in the U.S.— that’s heart disease. One in five women nationwide will die from coronary heart disease each year, and it’s often a silent killer: 65 percent of those who die will show no outward symptoms or may have had symptoms that were missed.
However, the good news is that 80-90 percent of all heart attacks and strokes can be prevented when patients are referred to a cardiologist early, and a routine screening mammogram can be part of that lifesaving equation. Multiple studies have shown a correlation between the presence of breast arterial calcifications (BAC) found in a mammogram and a higher risk of coronary heart disease (CHD), and the same groundbreaking AI used to improve breast cancer detection also allows doctors to detect these early signs of heart disease in the same mammograms used to screen for breast cancer.
Heart Health Month is an especially important time to focus on women’s health as a whole. Recently, four august doctors gathered on a virtual panel for Applied Radiology, and spoke about how AI can extend the value of mammograms by screening for both breast cancer and heart disease at once, and the way this holistic approach improves patient outcomes. These expert panelists in were:
Moderator:
- Dr. Nina Kottler, Associate Chief Medical Officer, Clinical AI, Radiology Partners (moderator)
- Dr. Kathy Schilling, Medical Director of Breast Imaging, Boca Raton Regional Hospital
- Dr. Heather Johnson, Preventive Cardiologist, Boca Raton Regional Hospital
- Dr. Fernando Collado-Mesa, Head of Innovation and Artificial Intelligence, Department of Radiology, University of Miami Miller School of Medicine
- Dr. Stamatia Destounis, Chair, Clinical Research and Medical Outcomes, Elizabeth Wende Breast Care
Webinar Recap
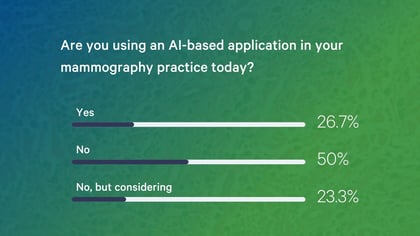
At the beginning of the webinar, participants were asked if they are using an AI-based application for mammography in their practice. Half of the participants said no, and the other half said that they were, or that they were considering it.
In addition, half of the participants said they reported breast arterial calcifications as part of their mammogram reading before the webinar—but this number jumped when attendees were repolled at the end of the session. After learning more about how AI can help detect early signs of heart disease, the number of participants who said they would plan on regularly reporting BAC as part of their mammogram readings jumped from 50% to 95%!
.jpg?width=420&name=Poll%20Questions%20for%20Feb%20Blog%20(2).jpg)
Here are the panelists’ answers to some of the top questions posed during the webinar.
What is the difference between CAD and AI CAD for breast imaging? What are the benefits of using AI to read a mammogram?
Dr. Schilling: CAD, or computer-aided detection software, was approved by the FDA in the late 1990s. It automatically marks suspicious areas in a mammogram but can only do so when it’s taught by humans exactly how to find them. With AI, the CAD software teaches itself how to spot suspicious areas in a mammogram and finds patterns physicians sometimes can’t detect. AI-based CAD will rank for the radiologist how suspicious a lesion is, while regular CAD will just say it’s “suspicious” without indicating how early or advanced a potential cancer might be. This is a huge help for a radiologist scrolling through dozens of mammogram images, because we’re human, we have long days, and we might not spot smaller, earlier cancers if we’re tired.
Dr. Destounis: AI provides that second pair of eyes for a double read, freeing doctors for other tasks. It essentially elevates radiologists, many of whom are not board-certified experts in breast imaging, to that specialist level because it uses deep learning to train itself on data from millions of other mammograms. Traditional CAD was not as good at detecting cancers earlier as we thought it might be and led to a lot of false positives and unnecessary workups. However, a radiologist’s expertise plus AI-based CAD is far better than either of them alone.
Is AI in breast imaging useful for modalities other than 2D mammography?
Dr. Johnson: Yes. The presence of breast arterial calcifications in a mammogram often correlates with early stages of heart disease, making it more likely that a patient could have a cardiovascular event like a heart attack or stroke within five years. In my experience, patients are grateful for the information when a radiologist alerts them to the fact that they have BAC and tells them about the associated risk of cardiovascular disease, so they can begin lifestyle changes and consult with a cardiologist.
Dr. Collado-Mesa: There is a growing interest in the correlation between BAC and heart disease in the breast imaging community. Most radiologists are aware of this growing evidence, but they do not always report the presence of calcifications as actual findings, simply because it’s not standard practice and they might be uncomfortable “stepping out of their lane.” However, women want to know about their heart disease risk if this information is available to them. I believe AI in breast imaging, and all of its uses, will change the way we work as radiologists.
Are there any correlations between BAC and carotid artery plaque?
Dr. Johnson: Carotid calcification can sometimes be associated with breast arterial calcifications, and aortic atherosclerotic disease too. In cardiology, there are female-specific cardiovascular risk factors like pregnancy-related high blood pressure, gestational diabetes, lupus, and rheumatoid arthritis. In my experience, women are more afraid of breast cancer than heart disease, but the fact that their doctor can see if they have BAC in their mammogram and can tell them why that means they’re at risk for heart disease, that mammogram gets them in the door to a cardiologist.
Have you found a correlation between BAC and breast density patterns?
Dr. Schilling: Not necessarily. However, because a patient’s breast density often affects how early breast cancer is detected, the same risk factors that might lead a patient to develop breast arterial calcifications that indicate heart disease are also risk factors for breast cancer. Many primary care providers and radiologists were initially resistant to reporting on breast density in a mammogram because they did not know about all the evidence for correlation. Now, it’s standard, and we have to teach radiologists and techs the importance of reporting the presence of BAC in a mammogram.
Once they know this option is available, many radiologists want to inform their patients about the presence of BAC but might be wary of “stepping out of their lane.” Any advice for radiologists who want to do this without alarming patients or calling for extra unnecessary exams from primary care providers?
Dr. Destounis: The emphasis should be on educating patients, letting them know that breast cancer screenings are important, but so is screening for heart disease, since that’s the number one killer of women in the U.S. Remember too that patients are already a little overwhelmed when you’re talking to them about breast cancer risk factors, so adding even more information about heart disease risk is a lot at once. For a radiologist, it’s helpful to identify cardiologists you can work with and refer patients to.
Dr. Schilling: We want women to be as passionate about cardiovascular health as their breast health, so it’s important to give them this information. It is helpful to be able to refer patients to a cardiologist willing and able to take on asymptomatic patients and advise them on lifestyle changes. We’re lucky to have Dr. Johnson, a preventive cardiologist, in our practice and available for those consultations. It’s also critical to educate your radiology techs, because they are the ones who spend the most time with patients—they need to be trained to tell patients exactly what we will be screening for in a mammogram, including breast arterial calcifications.
Dr. Johnson: It’s easier when you remember that all of us—radiologists, cardiologists, primary care physicians—are part of a team, and we all have the same goal: helping patients prevent their first cardiac event or halting the progression of cardiovascular disease. It’s also important to stress to patients that the presence of BAC isn’t necessarily an emergency, but also to keep the referring physician in the loop. If one of Dr. Schilling’s patients’ mammograms indicate the presence of BAC, they get a pamphlet explaining what it means, and giving them information to follow up with me or another cardiologist. It’s really about educating the patient, so they can ask the right questions to their primary care provider or a cardiologist about lifestyle changes. Patients are grateful for this information, and once their primary care physician realizes that this takes a burden off of them, they are as well.
One barrier to wider adoption of AI for mammography is reimbursement. When do you think Medicare might pay for the additional costs associated with AI-based CAD? What needs to happen for that to become a reality?
Dr. Destounis: As with traditional, non-AI CAD when it was first introduced, it could be years until we have the right codes. However, we can speed up the process if we have momentum behind the use of AI for mammography, and can prove widely that it has value, delivering results without significantly increased costs. It’s going to require education of patients, techs, radiologists, and referring doctors. Professional societies have to embrace and validate the use of AI, which would make it easier. We need an objective way to measure breast arterial calcifications and put it in perspective with a patient’s history and age.
One thing to remember is that patients have become more informed consumers as they have to pay more and more for their healthcare. New high deductible plans make women very aware of how much things cost. Radiology practices are publishing things like callback rates, statistics, and outcomes on their websites now. Patients and doctors alike need to know that AI means fewer callbacks, and if you get a callback, it’s more likely to be a real finding. With that in mind, until there’s more widespread reimbursement for it, women may even want to pay out of pocket for a mammogram ready using AI-based CAD, if they think it’s providing a service to them. Faster, more accurate results also mean the referring doctor is spared worried calls from patients who are waiting for results.
Dr. Collado-Mesa: The developers of these algorithms can keep in mind that AI can play a very important role in detecting, quantifying, and developing standardized reporting about the presence of BAC in a mammogram. This will make it easier in turn for radiologists to adopt and report and inform more research studies. Additionally, I think smaller AI companies have a major responsibility to prove to radiologists that this technology works, while making it easier for them to adopt. They need to work together a little more so they can have more data about how their algorithm works over a longer period of time, to make radiologists less anxious about incorporating AI for mammography into their practices.
Dr. Johnson: AI has the potential to be an extremely impactful tool for population health, preventing cardiac events by detecting asymptomatic heart disease early, and addressing barriers to care. If we’re able to screen for heart disease through the millions of mammograms conducted in the U.S. each year, it could be a game-changer. Yes, there is a lot of work to do as far as validation and looking at how BAC is detected by AI across populations, age groups, races/ethnicities and comorbidities. However, what’s most important is that patients want this information, and are more likely to use an imaging center that gives it to them.
Recent FDA analysis shows that they have cleared 39 AI algorithms for radiology in 2018, 49 in 2019, 88 in 2020 and 29 in 2021...does it not look like AI is a pandemic?
Dr. Kottler: If it’s a pandemic, it’s a good one, one that we want!
When doctors learn more about how it works, radiologists are overwhelmingly eager to adopt AI for mammography, and use it to report BAC. As one participant put it:
“It’s a great help both with workflow and finding early cancers. The women ARE coming [to our imaging center]. We love the AI. Thanks for your excellent discussion.”
Now that you've heard from the panelists and if processes were in place, do you plan on regularly reporting BAC as part of your mammogram reading?
Request a demo to learn more about how CureMetrix AI like cmAngio™ can help radiologists identify early signs of heart disease in a patient’s mammogram while improving their accuracy in detecting breast cancer.



